Content of
Rheumatoid Arthritis Disease Presentation
Slide 1: Introduction to Rheumatoid Arthritis Pathophysiology
- This title slide introduces a presentation focused on the underlying biological mechanisms of Rheumatoid Arthritis (RA).
- The design is clean and uses a vibrant purple color scheme.
- On the left, a prominent circular graphic features a hand under a magnifying glass, clearly illustrating the affected bone and joint structures.
Slide 2: Table of Contents – Rheumatoid Arthritis Pathophysiology
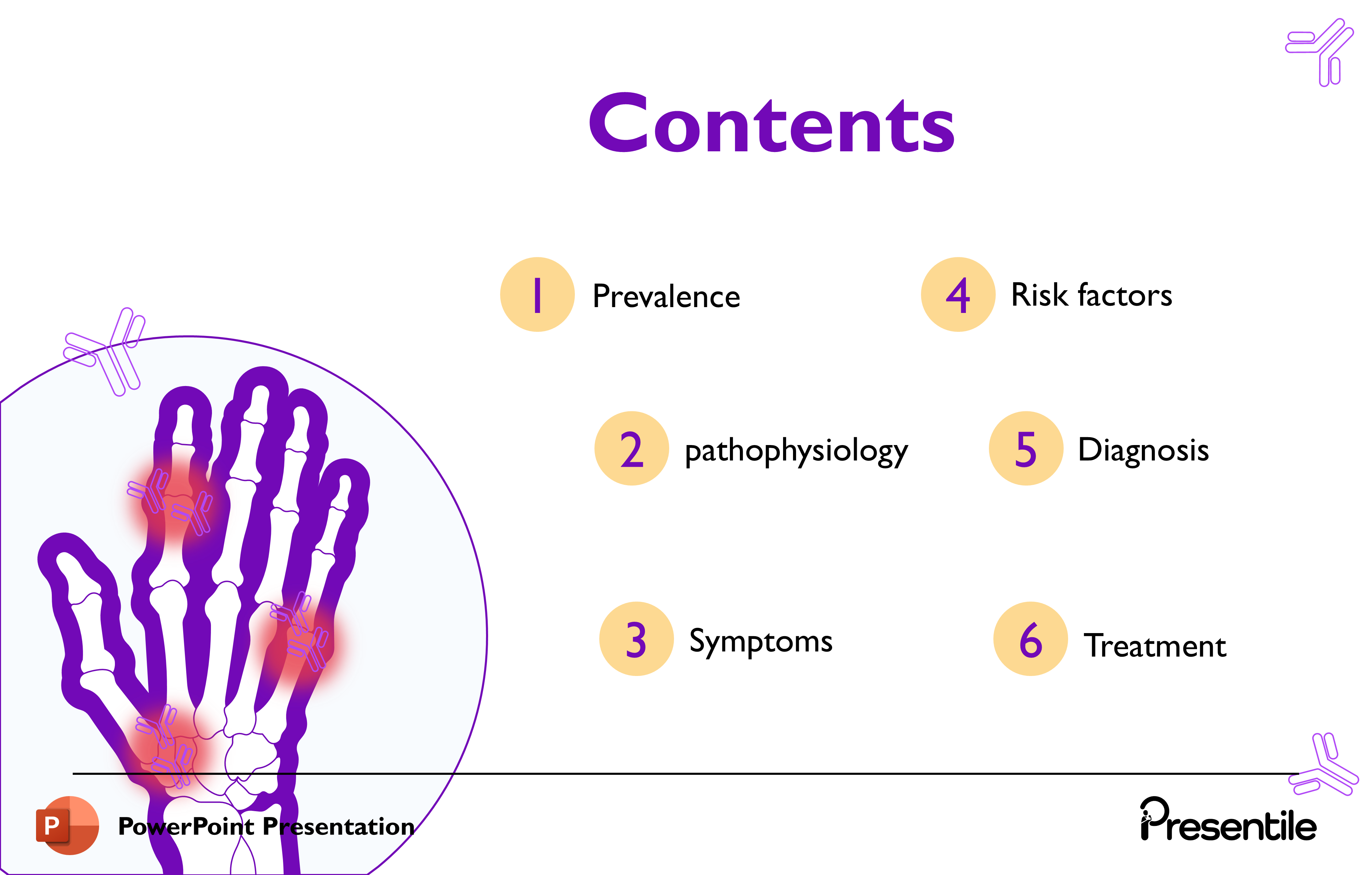
- This slide serves as the comprehensive agenda, outlining the six main topics that will be covered in the presentation.
- The design maintains the purple and yellow color scheme, with the prominent illustration of the affected hand and antibodies reinforcing the topic.
- The structured flow of the presentation is clearly laid out:
- Prevalence
- Pathophysiology
- Symptoms
- Risk factors
- Diagnosis
- Treatment
Slide 3: Defining Rheumatoid Arthritis
- This slide provides the fundamental definition of Rheumatoid Arthritis (RA).
- It uses a clear visual design, maintaining the purple and yellow color scheme, with the core anatomical illustration of the hand joints serving as the visual anchor.
- The definition is broken down into two key points:
- A chronic autoimmune disease in which the immune system mistakenly targets healthy tissues.
- The joints are most commonly affected, serving as the primary site of inflammation.
Slide 4: Facts about Rheumatoid Arthritis
.PNG)
- This slide uses the central image of the affected hand to visually tie the statistics to the disease's primary site.
- The key takeaways presented in the bubbles are:
- Etiology: The cause is a combination of genetic, environmental, or hormonal factors, establishing the multifactorial nature of the disease.
- Gender Disparity: Women are more likely to have rheumatoid arthritis.
- Ratio: The gender disparity is quantified, with a ratio of two to three women affected for every one man.
Slide 5: Global Prevalence of Rheumatoid Arthritis
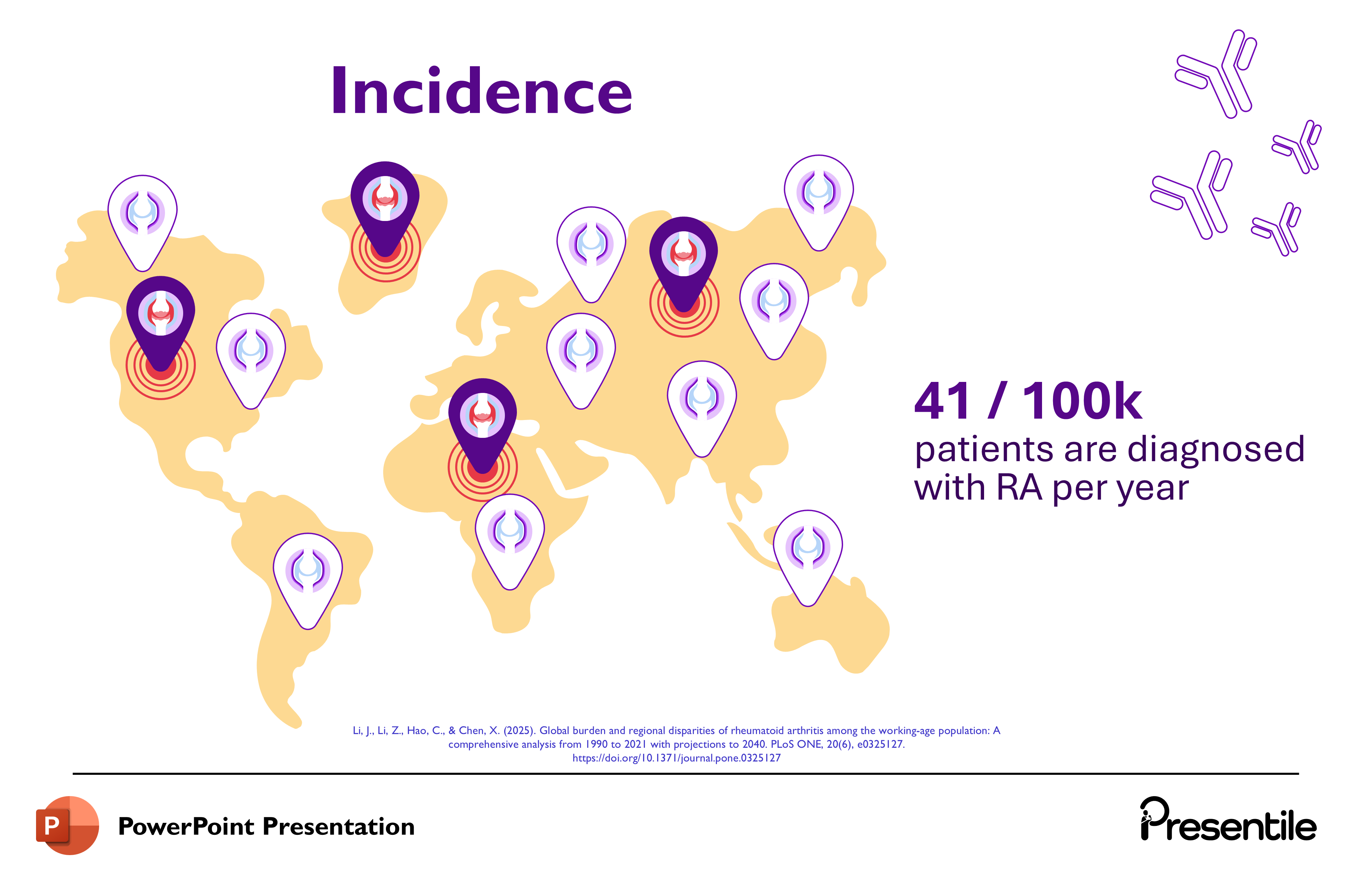
- This slide provides key statistics on the global burden of Rheumatoid Arthritis (RA).
- The central image is a world map covered with location markers, visually emphasizing the worldwide distribution of the disease.
- The key data points are:
- Global Case Count: In 2020, approximately 17.6 million individuals worldwide were diagnosed with RA.
- Prevalence Rate: The global prevalence rate is cited as 208 / 100K (per 100,000 individuals).
Slide 6: Section Focus: Pathophysiology of Rheumatoid Arthritis
- This slide serves as a clear, visually engaging transitional header for the Pathophysiology section.
- The word "Pathophysiology" is prominently displayed, signaling the shift in content focus.
- The visual elements, including the hand joint with inflamed areas and the small antibodies, are used to reinforce the core concepts of joint inflammation and autoimmune involvement, preparing the audience for a deep dive into the biological mechanisms of Rheumatoid Arthritis.
Slide 7: Detailed Pathophysiology – antibody Formation

- This slide begins the detailed explanation of the autoimmune process in Rheumatoid Arthritis.
- It focuses on the creation of the two signature autoantibodies, anti-CCP and Rheumatoid Factor (RF).
- Anti-CCP Antibody Formation (Point 1): Explains that IgG antibodies attack the cyclic citrullinated peptides (Citulline Antigens), resulting in the formation of the anti-CCP antibody. The visual clearly shows the IgG antibodies interacting with citrulline antigens and forming the anti-CCP structure.
- Rheumatoid Factor (RF) Formation (Point 2): Explains that IgM antibodies attack the IgG antibodies themselves, leading to the formation of rheumatoid factor (RF). The visual illustrates IgM attacking IgG to create the complex RF structure.
Slide 8: Pathophysiology – Antibody Migration to Joints
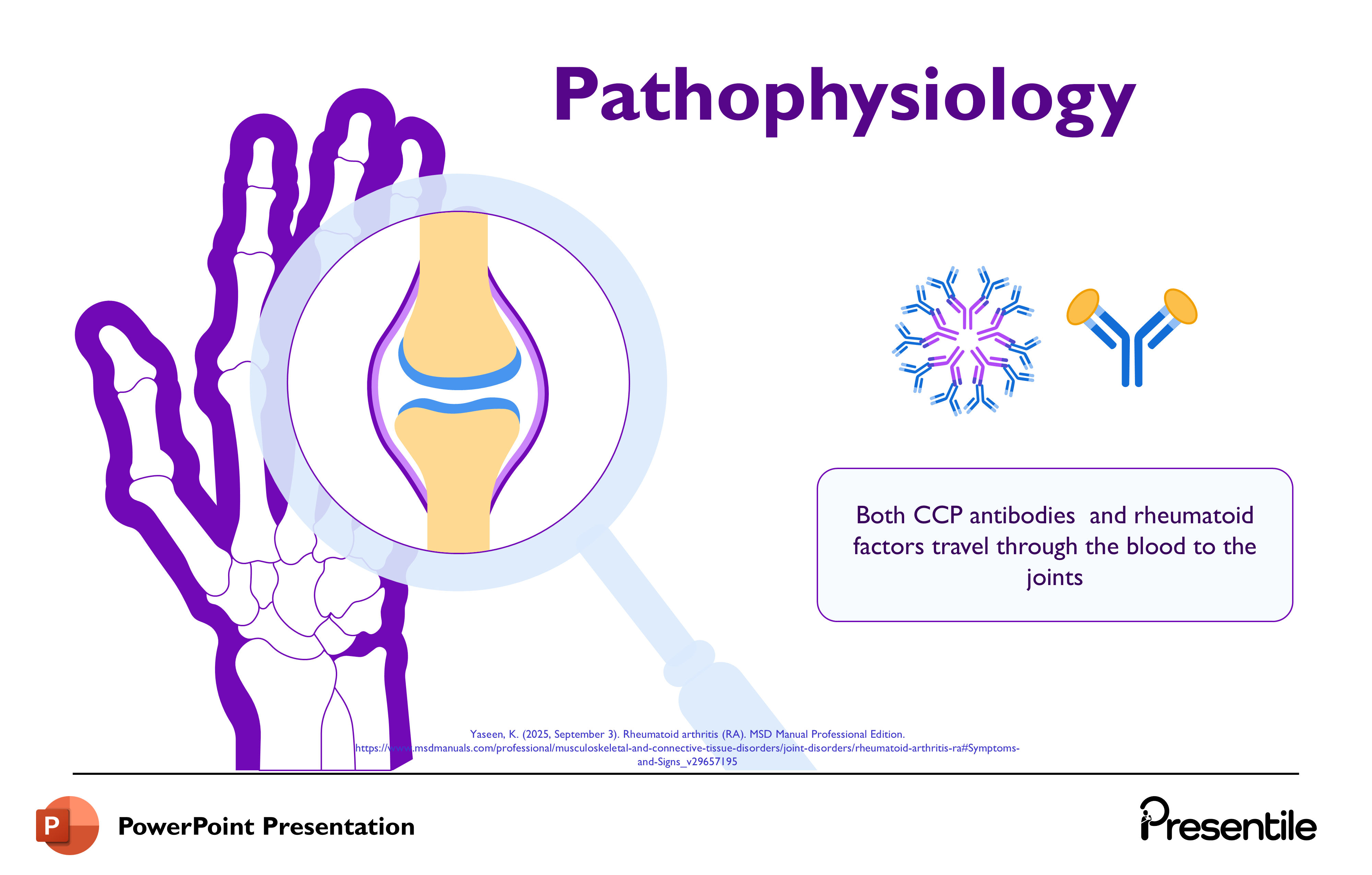
- This slide details the mechanism by which the autoimmune process translates into joint inflammation.
- It maintains the visual theme, using a magnified view of a healthy joint (synovial joint) surrounded by the purple hand outline and autoantibody graphics.
- The key message is that Both CCP antibodies and rheumatoid factors travel through the blood to the joints.
- This slide serves as the vital link between the molecular production of the antibodies (from the previous slide) and the site of clinical disease manifestation (the joint), setting up the next step of the inflammatory cascade within the joint itself.
Slide 9: Pathophysiology – Inflammatory Cascade and Cytokine Release
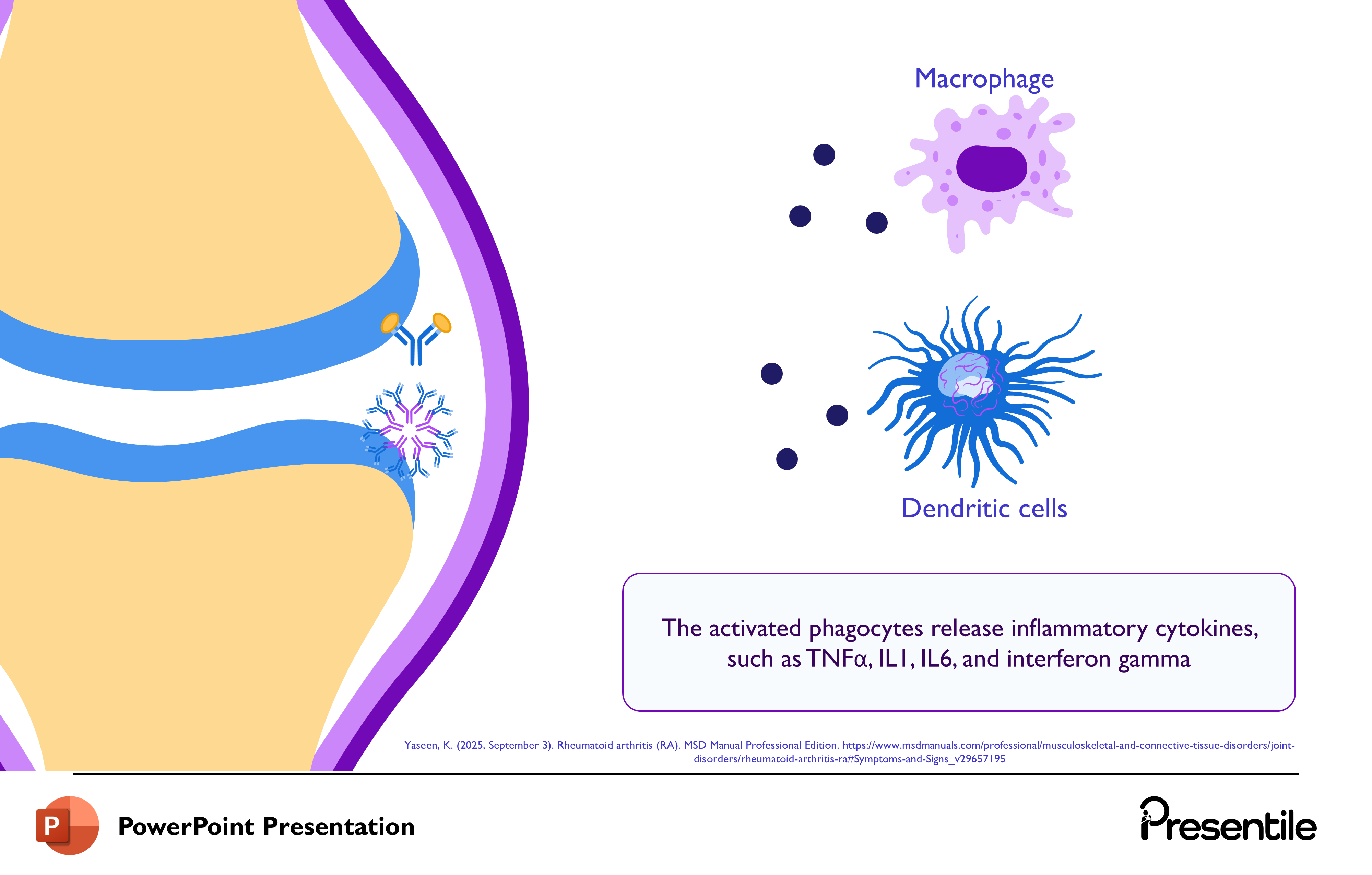
- This slide details the critical cellular events that follow the autoantibodies entering the joint space.
- It focuses on the activation of key immune cells (phagocytes) and the release of inflammatory mediators.
- The left side shows the autoantibodies (CCP and RF) residing within the joint's synovial fluid.
- The right side prominently displays two types of activated phagocytes: a Macrophage and a Dendritic cell.
- The central text explains that "The activated phagocytes release inflammatory cytokines, such as TNF\alpha, IL1, IL6, and interferon gamma."
Slide 10: Pathophysiology – Complement Activation and Neutrophil Recruitment
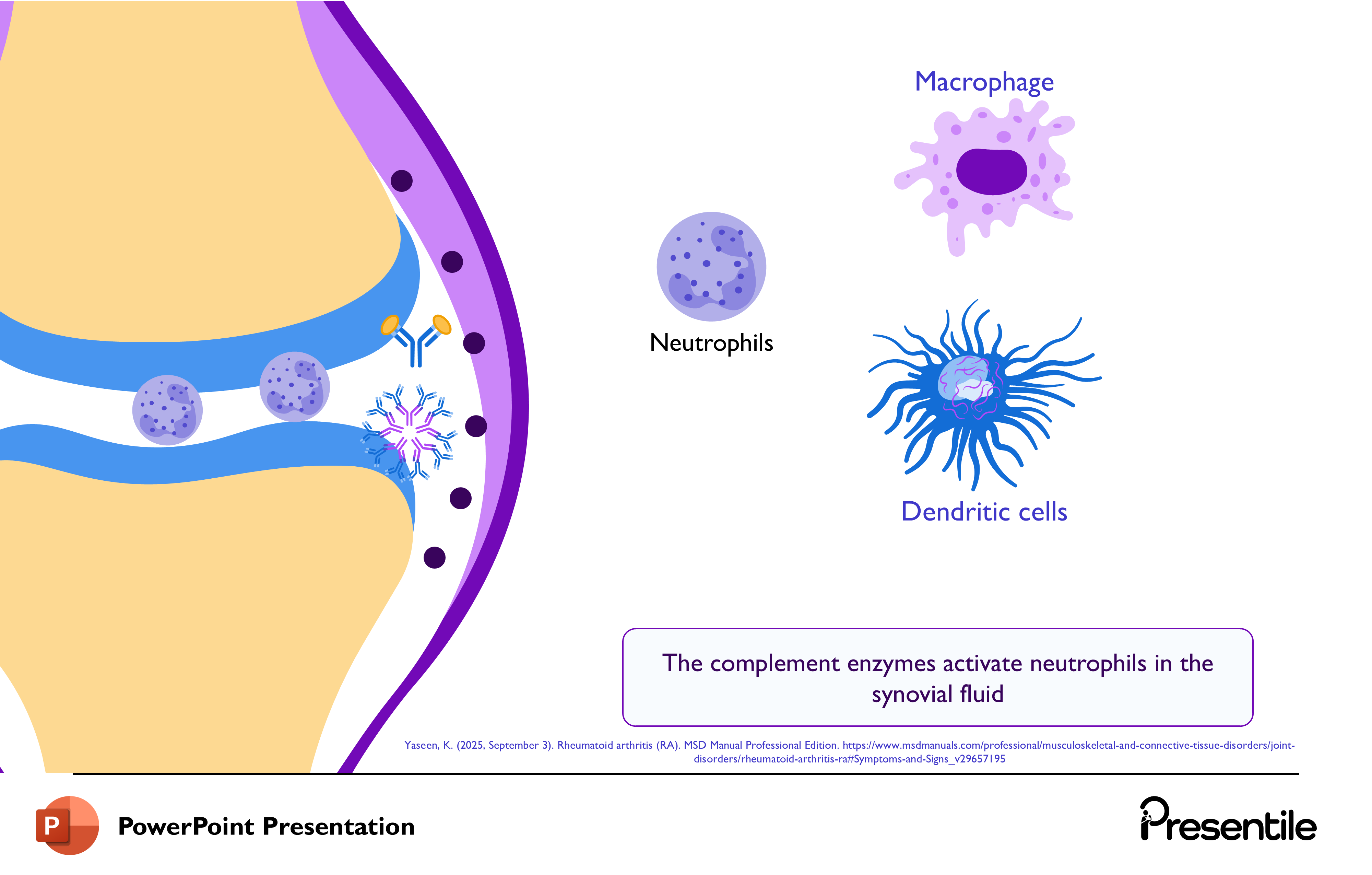
- This slide details the role of the complement system and neutrophils in the Rheumatoid Arthritis inflammatory process.
- The left side shows the autoantibodies (CCP and RF) bound within the joint capsule.
- Neutrophils are shown migrating into the synovial fluid. Macrophages and Dendritic cells remain on the right.
- The central text explains that "The complement enzymes activate neutrophils in the synovial fluid."
Slide 11: Symptoms of Rheumatoid Arthritis – Systemic and Joint Onset
This slide introduces the clinical symptoms of Rheumatoid Arthritis, focusing on the onset and overall effects.
- Visual Elements: The slide features a magnified view of a joint, indicating the primary site of disease, and an illustration of a person holding their inflamed ankle, representing the clinical manifestation.
- Key Points:
- "Systemic and joint manifestations of rheumatoid arthritis including cartilage and bone destruction occur." This highlights that RA is a whole-body (systemic) disease that causes permanent joint damage.
- "The onset of rheumatoid arthritis often begins with systemic and joint symptoms." This prepares the audience for a detailed look at the specific signs patients exhibit.
Slide 12: Key Clinical Symptoms of Rheumatoid Arthritis
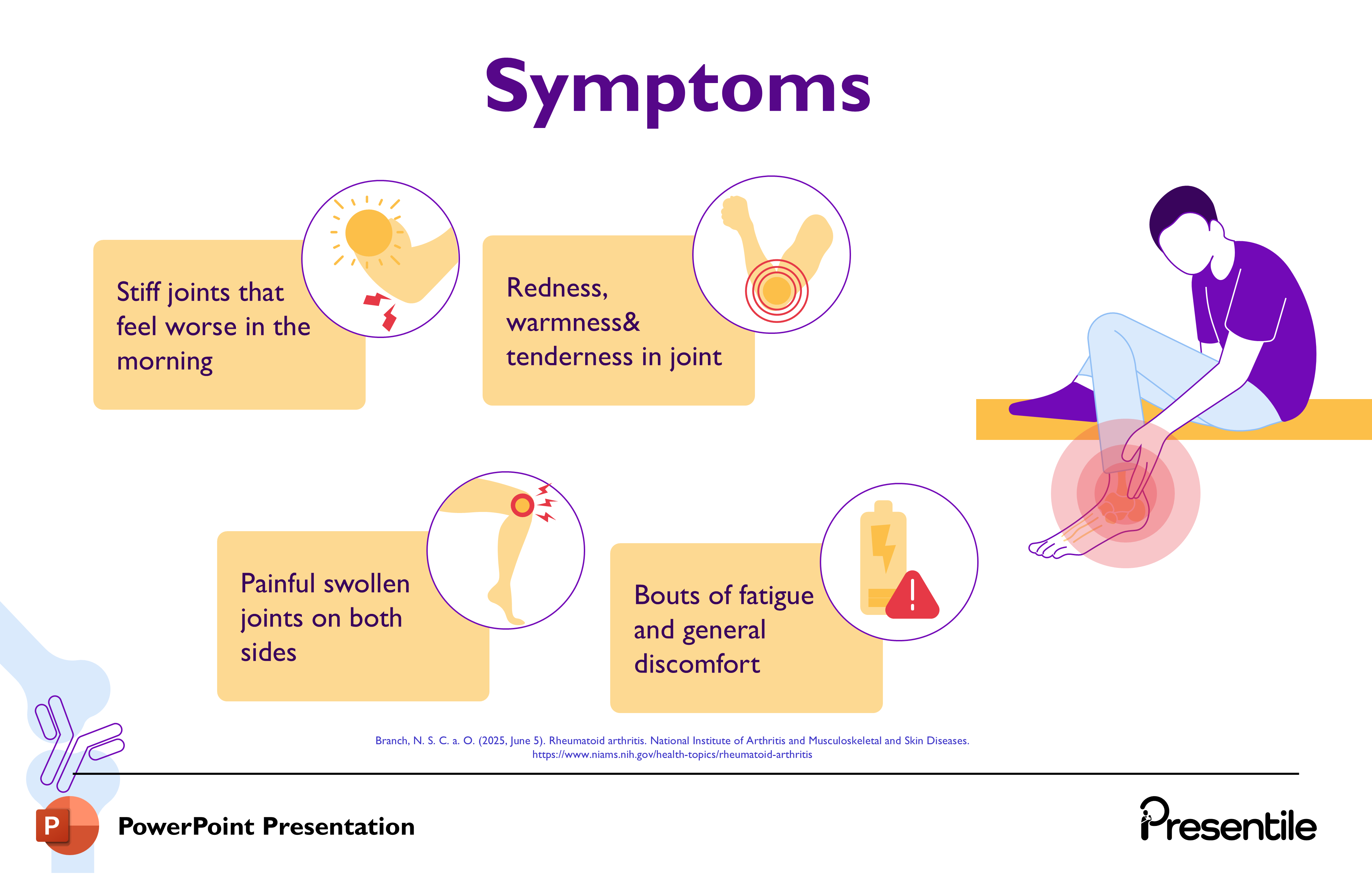
This slide provides a detailed breakdown of the four most common and telling clinical symptoms of Rheumatoid Arthritis (RA). The symptoms are visually paired with related graphics and arranged around the illustration of a person experiencing joint pain.
- Stiff joints that feel worse in the morning: This highlights the characteristic morning stiffness which improves throughout the day.
- Redness, warmness & tenderness in joint: These are the classic signs of acute inflammation within the affected joints.
- Painful swollen joints on both sides: This points to the symmetric and polyarticular nature of RA, a key diagnostic feature.
- Bouts of fatigue and general discomfort: This addresses the systemic symptoms of RA, emphasizing the profound general malaise that often accompanies the disease.
Slide 13: Key Risk Factors for Rheumatoid Arthritis
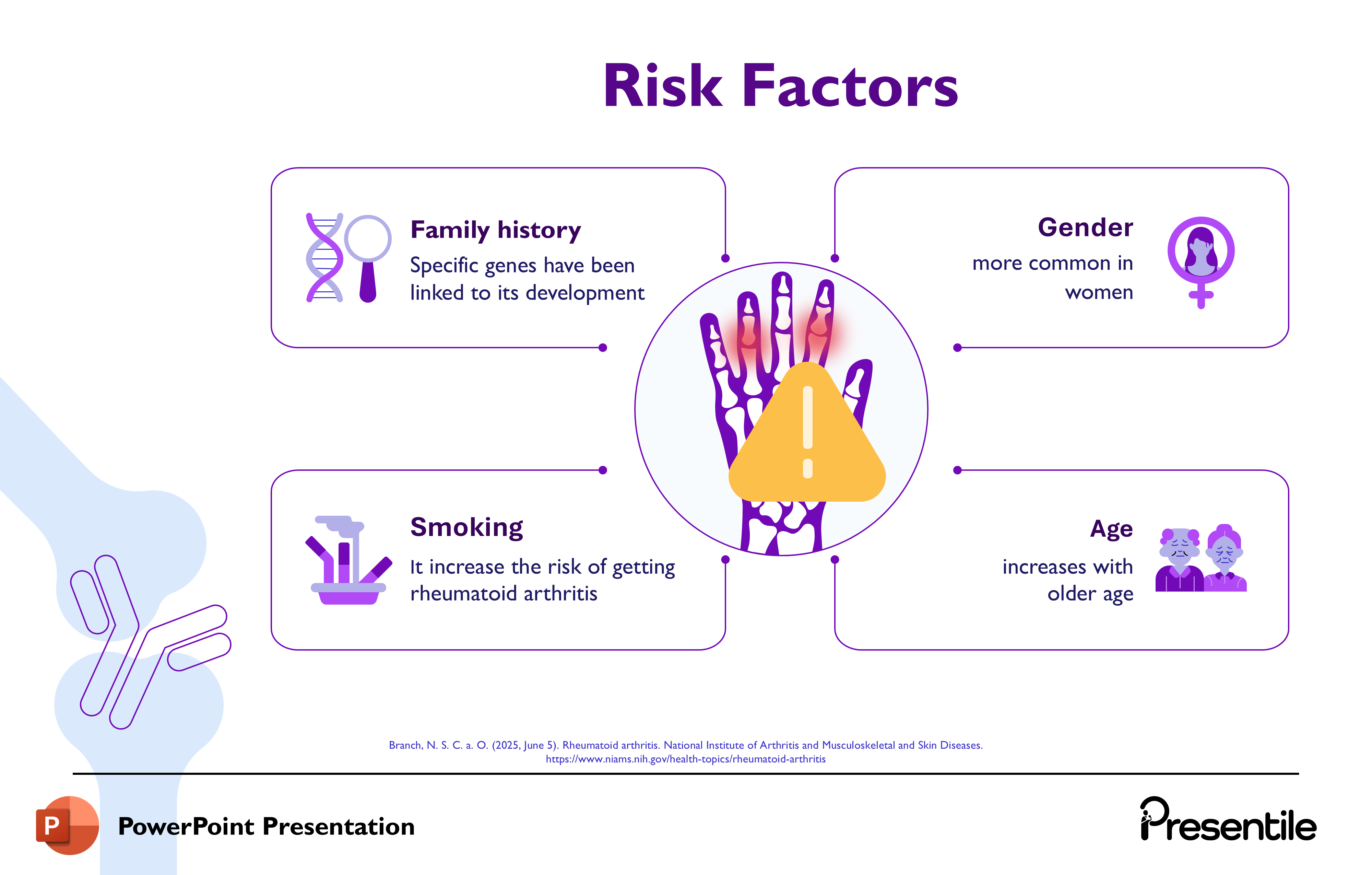
This slide details four major non-genetic risk factors that contribute to the development of Rheumatoid Arthritis (RA). The central image of the inflamed hand with a warning triangle emphasizes the potential risks.
- Family history: Notes that specific genes have been linked to its development, highlighting the genetic component.
- Gender: Re-emphasizes that RA is more common in women, which was introduced in the prevalence section.
- Smoking: States that it increases the risk of getting rheumatoid arthritis, pointing to a critical modifiable lifestyle factor.
- Age: Indicates that the risk increases with older age, showing a demographic factor for disease onset.
Slide 14: Section Focus: Diagnosis of Rheumatoid Arthritis

- This slide serves as a clear transitional header, signaling the shift in the presentation's focus to the methods used to identify and confirm Rheumatoid Arthritis (RA).
- The word "Diagnosis" is prominently displayed, accompanied by:
- The hand illustration, representing the primary clinical target.
- A test tube and clipboard, symbolizing the necessary lab work and clinical assessment.
Slide 15: Methods for Diagnosing Rheumatoid Arthritis
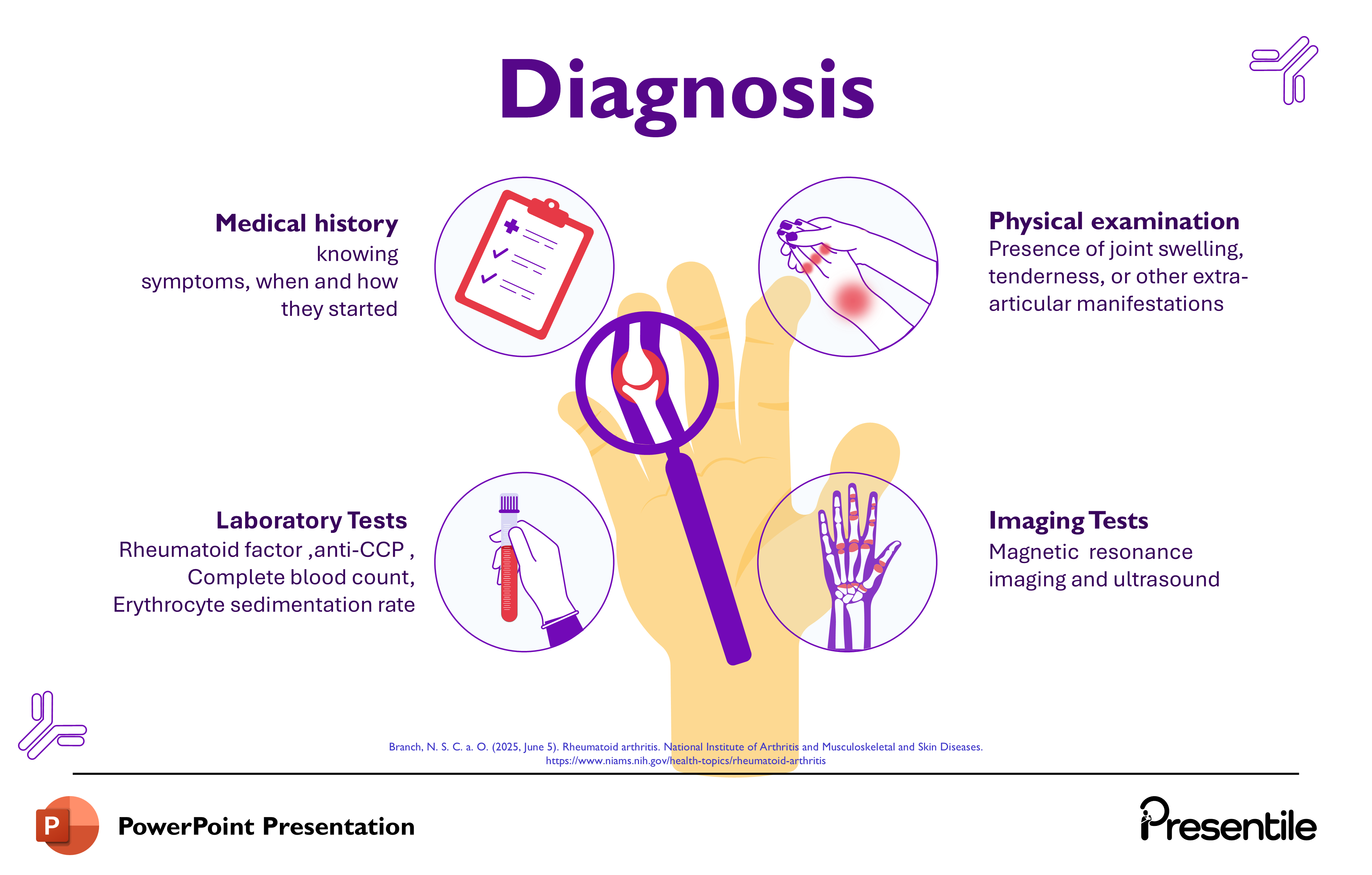
- This slide provides a comprehensive overview of the four essential components used to diagnose Rheumatoid Arthritis (RA).
- The central image of the hand under the magnifying glass links the diagnostic steps back to the primary site of disease. The four methods are presented in distinct circles:
- Medical history: Focuses on knowing symptoms, when and how they started, which is crucial for establishing the characteristic pattern of RA onset.
- Physical examination: Looks for the presence of joint swelling, tenderness, or other extra-articular manifestations, which confirms the clinical signs of active inflammation.
- Laboratory Tests: Lists key blood tests including Rheumatoid factor, anti-CCP, Complete blood count, and Erythrocyte sedimentation rate, which provide serological and inflammatory markers.
- Imaging Tests: Mentions Magnetic resonance imaging and ultrasound, which are used to visualize the extent of joint inflammation and damage.
Slide 16: Section Focus: Management (Treatment) of Rheumatoid Arthritis
%20of%20Rheumatoid%20Arthritis.PNG)
- This slide serves as the transitional header for the final section of the presentation, focusing on the treatment and management of Rheumatoid Arthritis (RA).
- The word "Management" is prominently displayed, which is an interchangeable term for treatment in this context.
- The accompanying visuals—the inflamed hand, a syringe, and a pill blister pack—immediately symbolize the medical interventions and pharmacology used to treat the disease.
Slide 17: Management – Medications and Physical Therapy

- This slide details the two primary categories of treatment for Rheumatoid Arthritis (RA): Medications and Physical Therapy.
- The design uses a circular layout, with the image of the affected hand at the center, symbolizing the target of the treatment.
- Medications: A list of key pharmaceutical treatments, essential for controlling the underlying autoimmune and inflammatory processes:
- Disease-modifying antirheumatic drugs (DMARDs)
- Biologic response modifiers (Biologics)
- Anti-inflammatory medications (like NSAIDs)
- Corticosteroids
- Physical Therapy: Describes the crucial non-pharmacological support: "Supports joint strength, flexibility, and functional independence."
Slide 18: Management – Joint Replacement Surgery
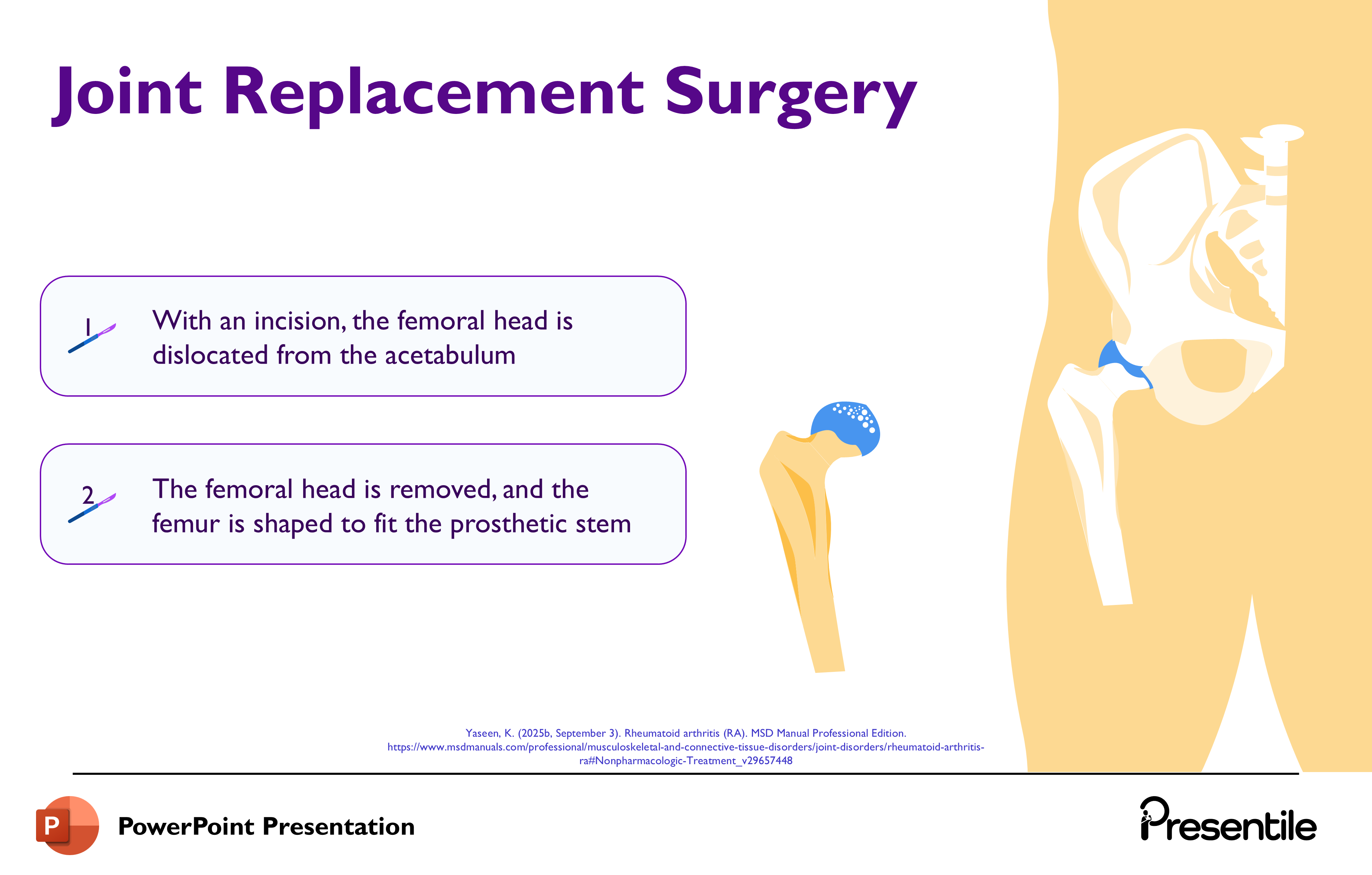
- This slide details the steps involved in Joint Replacement Surgery, a definitive treatment for advanced joint damage caused by Rheumatoid Arthritis.
- The focus is on a hip replacement, illustrating the mechanical steps of the procedure.
- Dislocation: "With an incision, the femoral head is dislocated from the acetabulum." This is the initial step to gain access to the damaged joint.
- Preparation and Resection: "The femoral head is removed, and the femur is shaped to fit the prosthetic stem." This prepares the bone to receive the implant components.
Slide 19: Management – Joint Replacement Surgery (Cont.)
.PNG)
- This slide details the remaining steps of the Joint Replacement Surgery, focusing on the fixation and final assembly of the prosthetic hip joint.
- Step 3 (Acetabular Component Fixation): "The acetabular component is fixed to the hip bone." This involves securing the cup-shaped component into the pelvis.
- Step 4 (Fixation): "Screws or bone cement are used for fixation." This explains the mechanism used to permanently secure the prosthetic components to the natural bone.
- Step 5 (Femoral Head Attachment and Reduction): "The prosthetic femoral head is attached to the stem and reduced into the acetabular component." This is the final step, where the new ball joint is inserted into the new socket, completing the replacement.
Slide 20: Thank You and Conclusion

- This slide serves as the professional and friendly conclusion to the presentation.
- The prominent "Thank You" message provides a clear final sign-off. The circular graphic featuring the inflamed, affected hand, along with a purple and blue ribbon (often used to represent RA awareness), reinforces the topic and the seriousness of the disease.
Features of
Rheumatoid Arthritis Disease Presentation
- Fully editable in PowerPoint
- All graphics are in vector format
- Medically Referenced information and data
Specifications
 Slides count:
Slides count: Compatible with:Microsoft PowerPoint
Compatible with:Microsoft PowerPoint File type:PPTX
File type:PPTX Dimensions:16:9
Dimensions:16:9
Elevate Your Work with Our Innovative Slides
Thank you! Your submission has been received!
Oops! Something went wrong while submitting the form.
No items found.