Content of
Heart Failure Presentation
Slide 1: Heart Failure (Title Slide)
.PNG)
This slide introduces a critical presentation on Heart Failure, a serious condition where the heart cannot pump blood efficiently.
- Title: The topic, Heart Failure, is clearly and boldly presented.
- The slide features a prominent illustration of a human heart , complete with vessels, and includes a warning sign/exclamation mark to immediately convey the severity and seriousness of the condition.
- The background uses a light blue and white color scheme with a few soft blue squares, creating a clean, yet serious, visual tone.
Slide 2: Introduction

This slide serves as the introduction and transition from the title slide to the core content of the presentation.
- The slide simply displays the word "Introduction" in large blue letters , framed within a simple blue border.
- The heart icon remains on the left, reinforcing the topic established on the title slide.
Slide 3: What is Heart Failure? (Definition)
.PNG)
This slide provides the concise physiological definition of Heart Failure (HF), emphasizing the heart's failure as a pump.
- Definition: "The heart's impaired pumping function fails to meet the body's circulatory demands". This clarifies that HF is not a sudden cessation of the heartbeat (like cardiac arrest), but rather a chronic inability to maintain adequate circulation.
- Visual Elements:
- A graphic of the chest cavity shows the heart and pulmonary circulation , visually representing the system that is under strain in heart failure.
- A progress bar at the top indicates the current section (Definition) while showing the subsequent sections: Signs & Symptoms and Classification.
Slide 4: Signs & Symptoms
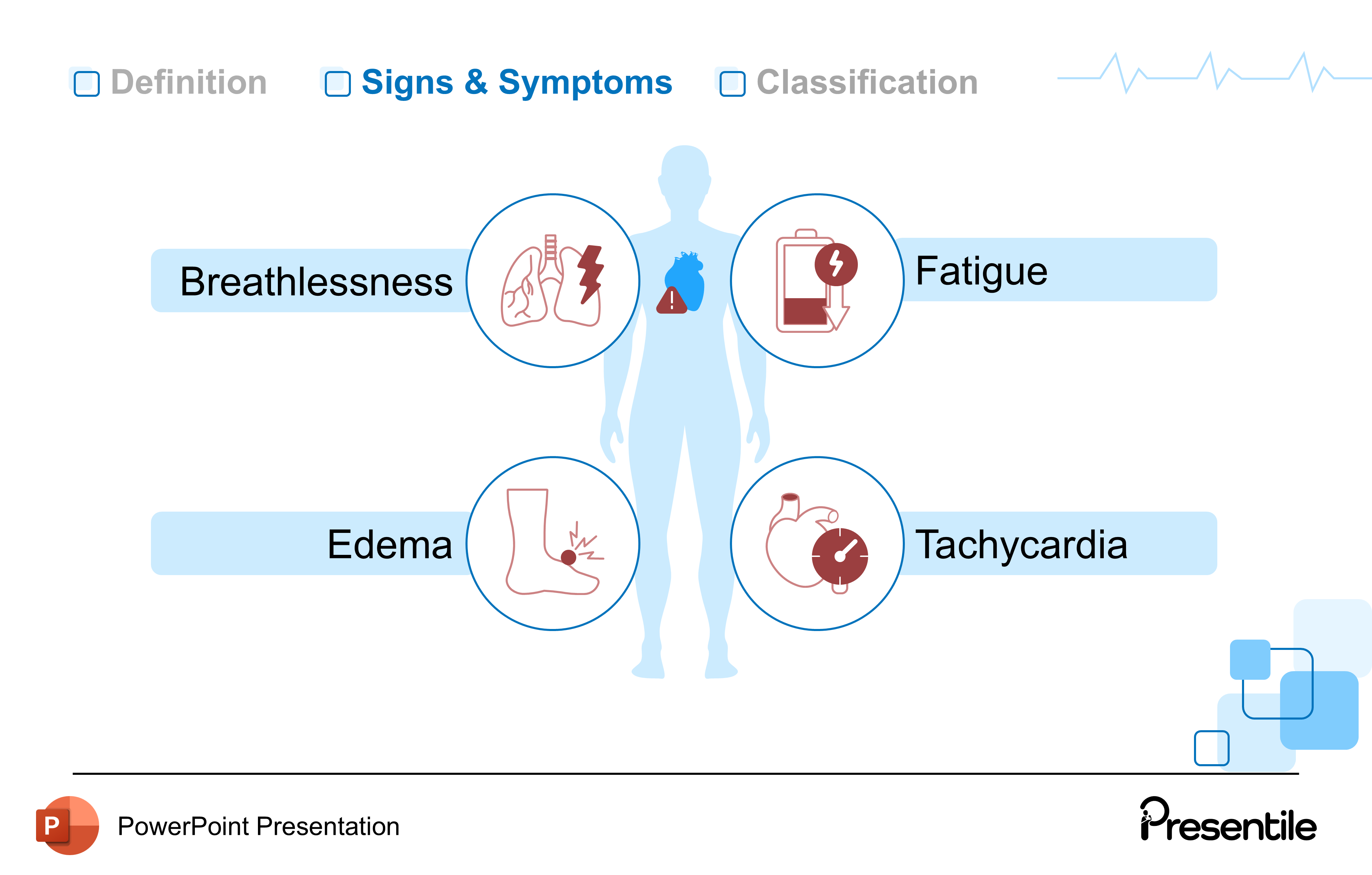
This slide details four major clinical manifestations of Heart Failure, which result from the heart's impaired pumping ability and subsequent fluid backup. The progress bar at the top indicates we are now in the Signs & Symptoms section.
- Breathlessness (Dyspnea): Often linked to pulmonary edema (fluid backing up into the lungs) due to left-sided heart failure .
- Fatigue: Caused by the heart's failure to supply enough oxygenated blood to the body's tissues .
- Edema (Swelling): Particularly in the legs and ankles, caused by fluid backing up into the systemic circulation due to right-sided heart failure .
- Tachycardia: A compensatory mechanism where the heart beats faster in an attempt to pump more blood to meet the body's demands .
Slide 5: Classification (AHA/ACC Stages)
.PNG)
This slide introduces the four stages of the American Heart Association (AHA) and American College of Cardiology (ACC) classification system for Heart Failure. This staging system is Important because it focuses on the development and progression of the disease, allowing for intervention even before symptoms appear.
The slide highlights the Classification section.
- Stage A: "At risk for HF"
- Applied to asymptomatic patients with risk factors (e.g., hypertension, diabetes). The heart structure is still normal.
- Stage B: "Pre-HF"
- Adds cardiac structural changes (e.g., reduced ejection fraction, enlargement) still in the absence of symptoms.
- Stage C: "Symptomatic HF"
- Structural disease with current or previous symptoms (like the ones detailed on the previous slide). This is the traditional definition of Heart Failure.
- Stage D: "Advanced HF"
- Severe debilitating symptoms or repeated hospitalizations despite optimal medical therapy.
Slide 6: Pathophysiology (Heading)
.PNG)
This slide serves as a heading to transition the presentation from the clinical definition and classification to the underlying physiological mechanisms of Heart Failure.
- The slide prominently displays the word "Pathophysiology" to indicate the shift in focus.
- The image of interlocked gears and the stylized heart icon convey the idea of complex, interrelated mechanisms (or "gears") that are at the root of the disease.
Slide 7: Pathophysiology (Compensatory Mechanisms)
.PNG)
This slide introduces the initial, short-term mechanisms the body uses to try and compensate for the heart's failing function.
The content lists the three primary mechanisms, with the first one expanded upon:
- Frank-Starling Mechanism: This is a key principle of cardiac physiology. It is defined here as "Increased ventricular preload to sustain cardiac output". Essentially, the heart stretches more to increase the force of contraction.
- Hypertrophic Remodeling: The heart muscle attempts to adapt by thickening its walls. (Mentioned but not detailed)
- Neurohumoral Activation: The body activates hormonal systems (like the Renin-Angiotensin System) to maintain blood pressure and volume. (Mentioned but not detailed)
- The center graphic shows a cardiac muscle cell , representing the structural component involved in the Frank-Starling mechanism, which is connected to the whole heart diagram.
Slide 8: Pathophysiology (Hypertrophic Remodeling)
.PNG)
This slide details the structural change that occurs in the heart muscle in response to chronic stress, known as Hypertrophic Remodeling.
- Hypertrophic remodeling is defined as the "Thickening of the ventricular wall to handle increased stress".
- This thickening initially helps the heart pump against high pressure (e.g., from hypertension) or pump a high volume of blood, but eventually leads to reduced chamber volume and stiffness, impairing heart function.
- The heart diagram shows the hypertrophied (thickened) ventricular wall, visually demonstrating the consequence of this remodeling.
Slide 9: Pathophysiology (Neurohumoral Activation)
.PNG)
This slide details the body's hormonal and nervous system response to a failing heart, which is a key target for modern heart failure therapies.
- Neurohumoral Activation occurs when the failing heart triggers the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system (SNS).
- While initially helpful in the short term (e.g., maintaining blood pressure), chronic activation of the RAAS and SNS is actually detrimental, causing vasoconstriction, fluid retention, and further damage/remodeling to the heart muscle.
- The diagram shows the acronyms RAAS and SNS pointing to a constricted blood vessel and the heart, illustrating the systemic and cardiac effects of this activation.
Slide 10: The Downward Spiral of Heart Failure
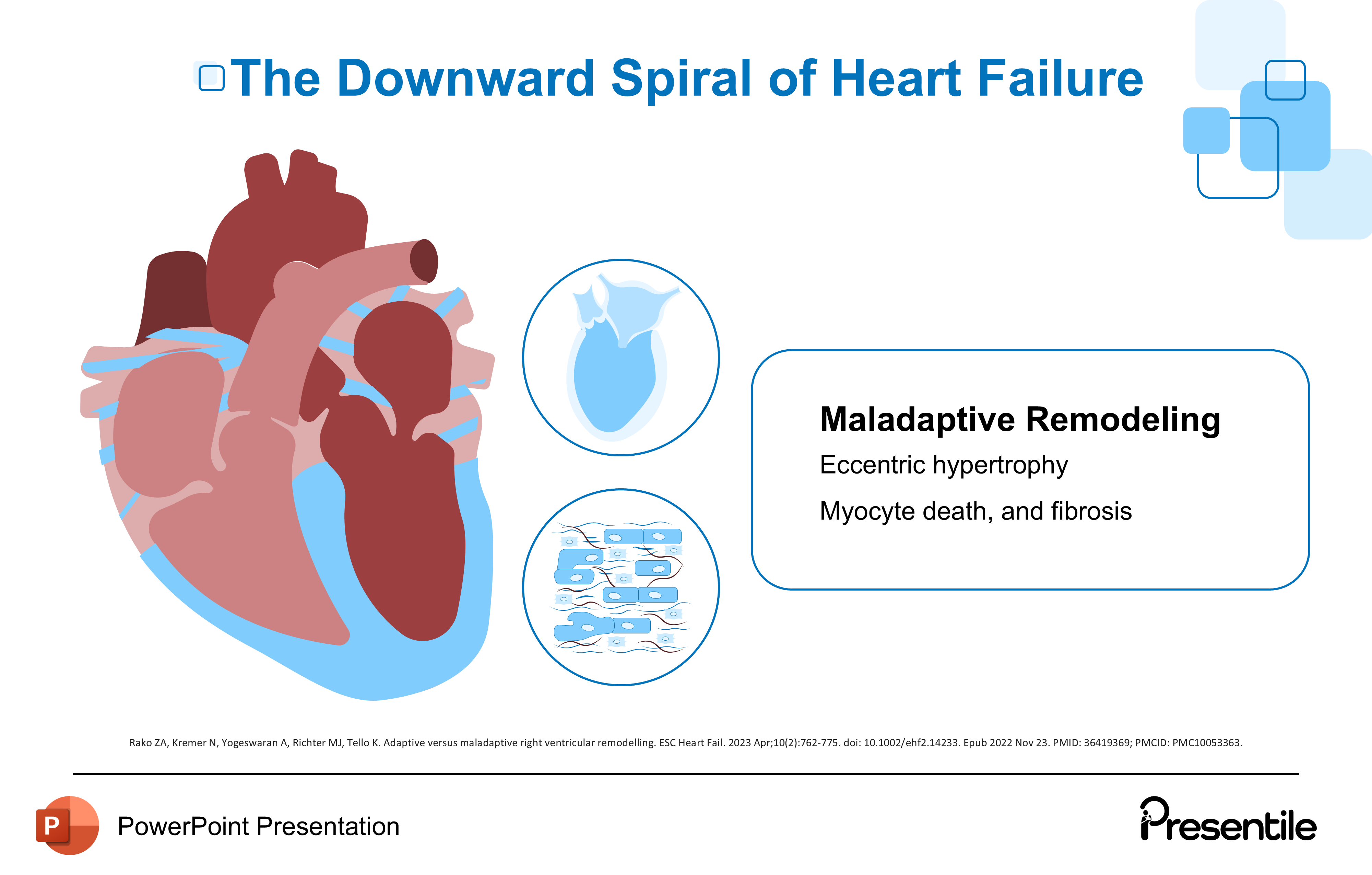
This slide details the detrimental phase of Heart Failure pathophysiology, where the initial compensatory mechanisms become harmful, leading to structural and functional deterioration.
- The title "The Downward Spiral of Heart Failure" emphasizes the progressive and destructive nature of chronic heart failure.
- This spiral leads to Maladaptive Remodeling.
- Eccentric hypertrophy: This is a type of remodeling where the heart chambers enlarge and stretch, rather than just thickening.
- Myocyte death, and fibrosis: The chronic stress and neurohumoral activation cause heart muscle cells (myocytes) to die and be replaced by non-contractile scar tissue (fibrosis).
- The large heart diagram shows an enlarged, stretched left ventricle, which visually represents eccentric hypertrophy, while the magnified image shows damaged myocyte cells and scar tissue.
Slide 11: The Downward Spiral of Heart Failure (Neurohormonal Overload)
.PNG)
This slide provides a detailed explanation of how the chronic activation of the neurohormonal systems (introduced on Slide 9) contributes to the destructive phase of heart failure.
- The overactivation of the RAAS (Renin-Angiotensin-Aldosterone System) and SNS (Sympathetic Nervous System) leads to Neurohormonal Overload.
- Consequences: This overload causes vasoconstriction (narrowing of blood vessels) and sodium retention, which ultimately increase the cardiac afterload. Afterload is the pressure the heart must pump against, and increasing it further stresses the already failing heart.
- The diagram explicitly shows the heart, a constricted vessel, and the kidney retaining sodium (Na), visually linking the RAAS/SNS activation to the systemic consequences.
Slide 12: The Downward Spiral of Heart Failure (Calcium Overload)
.PNG)
This slide details the detrimental effects of altered calcium handling within the heart muscle cells, a key process in the final, destructive phase of heart failure.
- Calcium Overload leads to a host of problems:
- Arrhythmias: Disrupted calcium cycling contributes to abnormal electrical activity.
- Impaired relaxation: The heart muscle cannot relax fully between beats (diastolic dysfunction).
- Increased energy demand: The faulty calcium cycle requires more energy from the struggling heart.
- The heart diagram shows calcium ions (Ca) cycling within the heart chambers , illustrating the cellular problem at a macroscopic level.
Slide 13: The Role of Neurohormones
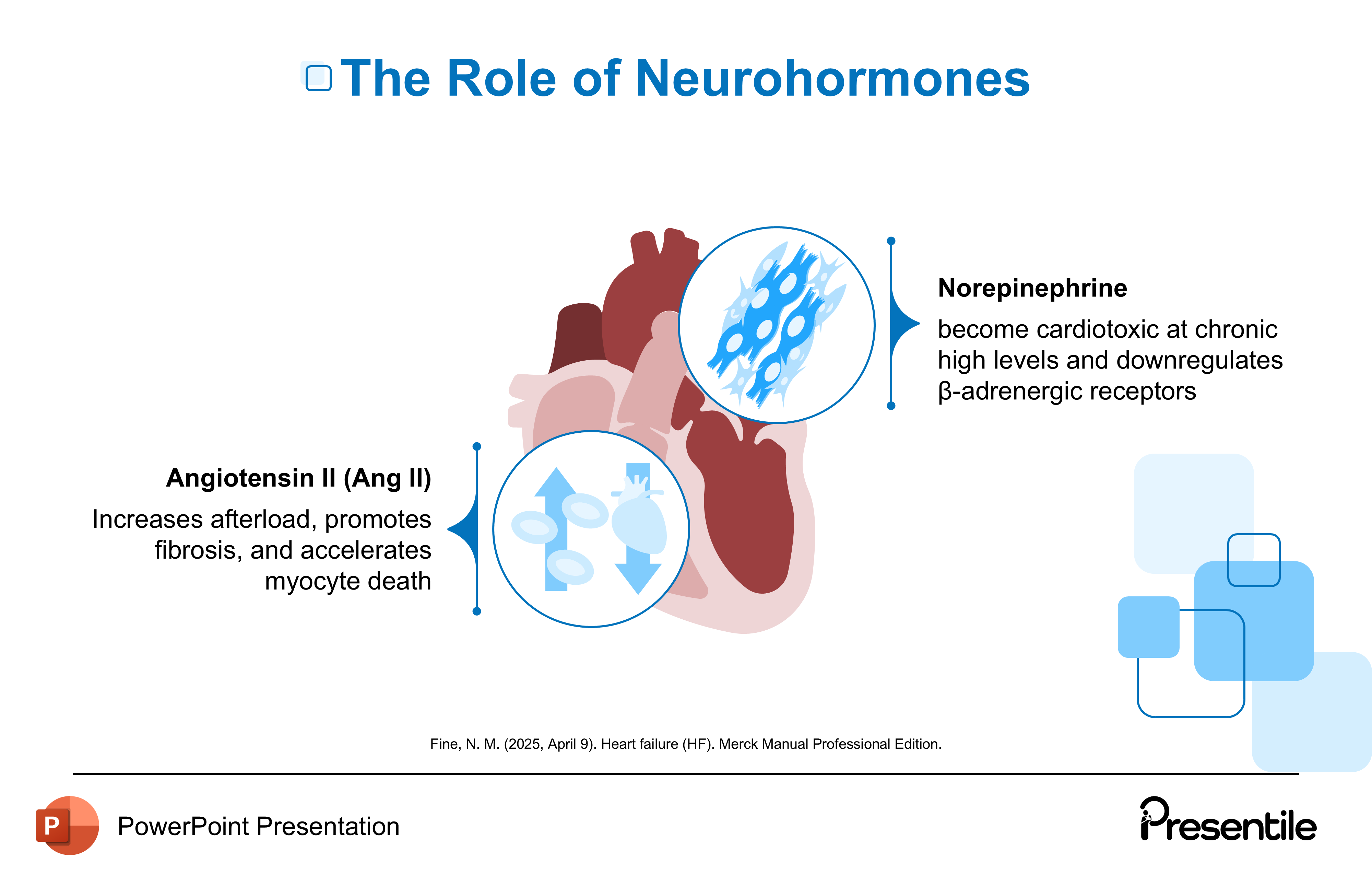
This slide breaks down the specific detrimental effects of the two key neurohormones—Angiotensin II and Norepinephrine—in the context of chronic heart failure. This is a critical slide for understanding pharmacological treatments.
- Angiotensin II (Ang II):
- Increases afterload.
- Promotes fibrosis (scar tissue formation).
- Accelerates myocyte death (heart muscle cell death).
- Medications like ACE inhibitors and ARBs directly target this pathway.
- Norepinephrine:
- Becomes cardiotoxic (poisonous to the heart) at chronic high levels.
- Downregulates β-adrenergic receptors. This means the heart becomes less responsive to the body's own adrenaline, which is part of the heart's overall functional decline.
- Beta-blockers directly target this pathway.
Slide 14: Systolic vs Diastolic Heart Failure
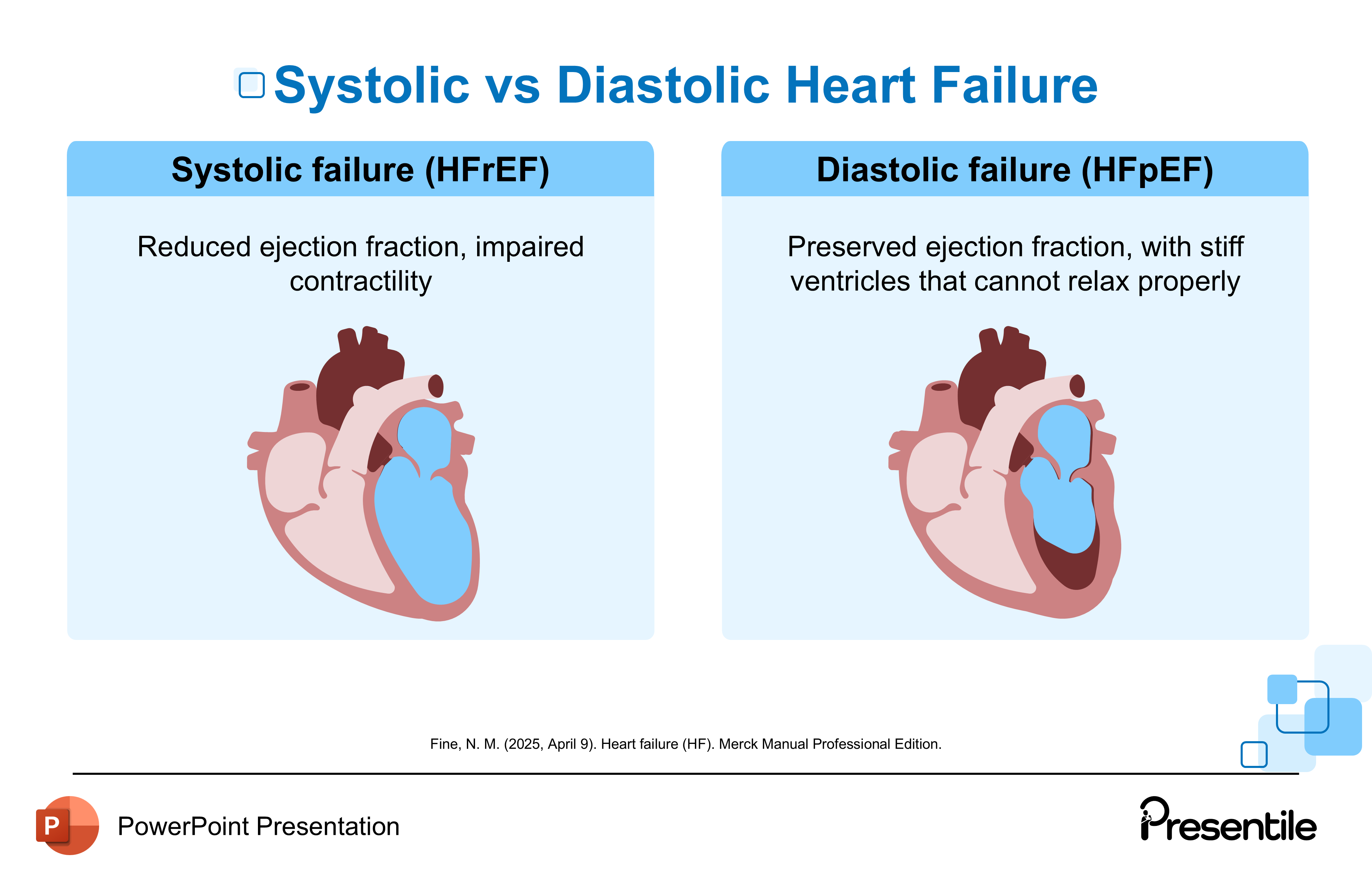
The slide introduces the modern classification of heart failure based on the heart's pumping efficiency, which is measured by Ejection Fraction (EF). This distinction is vital because the treatment approach for each type is very different.
- Systolic failure (HFrEF):
- Characterized by Reduced ejection fraction, impaired contractility.
- HFrEF is often viewed as a "squeezing" problem where the heart cannot effectively push blood out.
- Diastolic failure (HFpEF):
- Characterized by Preserved ejection fraction, with stiff ventricles that cannot relax properly.
- HFpEF is a "filling" problem where the heart cannot adequately fill with blood between beats due to stiffness.
- The slide uses two diagrams of the heart to contrast the two states: the HFrEF heart looks stretched and dilated, while the HFpEF heart looks thick-walled and stiff, visually capturing the difference in ventricular mechanics .
Slide 15: Diagnosing Heart Failure
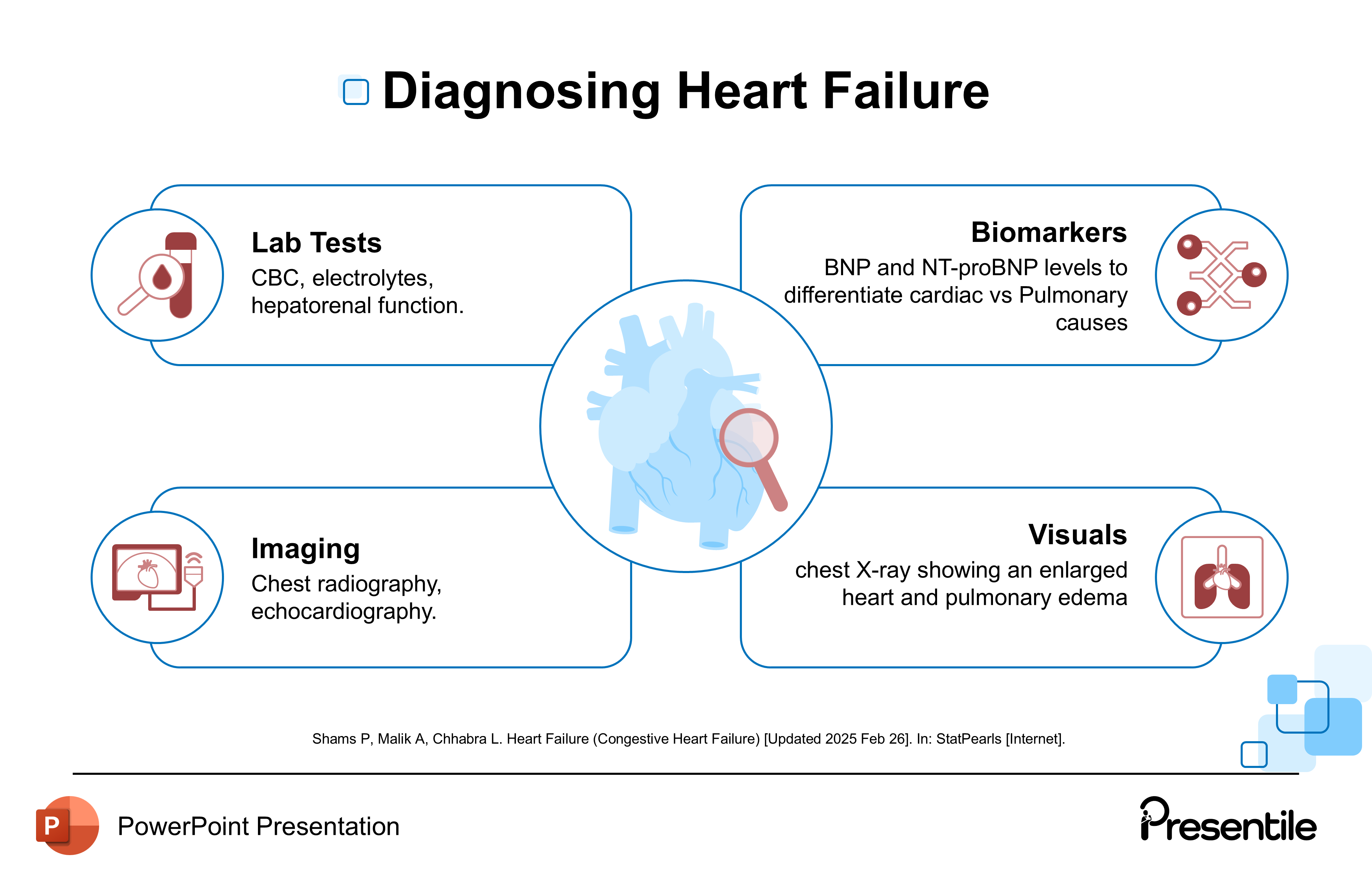
This slide provides a comprehensive overview of the four key diagnostic pillars used to confirm Heart Failure and determine its cause and severity.
- Lab Tests: Includes screening for CBC (Complete Blood Count), electrolytes, and hepatorenal function (liver and kidney function).
- Biomarkers: Assesses BNP (Brain Natriuretic Peptide) and NT-proBNP levels. These markers help differentiate cardiac vs. pulmonary causes of symptoms like shortness of breath.
- Imaging: Utilizes chest radiography and echocardiography. Echocardiography is particularly important for measuring the Ejection Fraction (EF) to classify the type of HF (HFrEF vs. HFpEF).
- Visuals: In the case of severe Heart Failure, visuals like a chest X-ray may show an enlarged heart and pulmonary edema (fluid in the lungs).
Slide 16: Complications
This slide details the five major long-term complications and comorbidities associated with chronic Heart Failure, highlighting the systemic nature of the syndrome.
- Risk of thromboembolism: Blood clots can form due to sluggish blood flow in the heart, leading to a risk of stroke or pulmonary embolism.
- Recurrent hospitalizations: Heart Failure is a chronic condition frequently leading to flare-ups (decompensation) requiring hospital admission.
- Cardiorenal disease: Also known as cardiorenal syndrome, this refers to the complex interaction where the failing heart further damages the kidneys and vice-versa.
- Liver dysfunction: Fluid congestion backing up into the liver (congestive hepatopathy) can impair liver function.
- Reduced quality of life: The chronic symptoms (fatigue, breathlessness) significantly impact the patient's daily activities and well-being.
Slide 17: Heart Failure Management
This slide details the three major components of modern Heart Failure therapy, ranging from basic lifestyle changes to advanced pharmacological treatments. This is the crucial, actionable final content slide.
- Lifestyle Changes: This is the foundational element, including Sodium and fluid restriction, weight monitoring, and tailored physical activity.
- Core Medications: These are the established drug classes that form the basis of treatment for HFrEF:
- Diuretics
- ACE inhibitors
- ARBs (Angiotensin II Receptor Blockers)
- Beta-blockers
- MRAs (Mineralocorticoid Receptor Antagonists)
- Advanced Therapies: These newer or specialized treatments offer further benefit, often for patients with more severe disease:
- ARNIs (Angiotensin Receptor-Neprilysin Inhibitors)
- SGLT2 inhibitors
- Inotropes for symptom relief
Slide 18: Tackling Comorbidities

This slide focuses on five major comorbidities that frequently occur alongside, and often worsen, Heart Failure. Successfully managing these conditions is critical for improving patient outcomes.
- Coronary artery disease: This is a major cause of HF and is a crucial comorbidity to manage.
- Valvular heart disease: Issues with the heart valves can worsen the heart's pumping function and increase strain.
- Anemia: Low red blood cell count (Anemia) places extra strain on the heart, forcing it to pump harder to deliver oxygen.
- Sleep apnea: This condition is strongly linked to HF and contributes to the chronic stress on the cardiovascular system.
- Atrial fibrillation: This is a common arrhythmia in HF patients that impairs ventricular filling and contributes to the progression of the disease.
Slide 20: Advanced Interventions
This slide details advanced, non-pharmacological interventions for Heart Failure, including procedures, devices, and transplantation. The inclusion of this slide right before the conclusion highlights the complexity of care for advanced disease.
- Revascularization: Includes procedures like CABG (Coronary Artery Bypass Graft) and PCI (Percutaneous Coronary Intervention) for ischemic heart failure. This addresses the underlying coronary disease.
- Devices: These are implantable technologies used to support heart function: CRT (Cardiac Resynchronization Therapy), ICDs (Implantable Cardioverter-Defibrillators), and VADs (Ventricular Assist Devices).
- Transplantation: This is described as the gold standard for end-stage heart failure.
Slide 21: Thank You (Conclusion)
.PNG)
This is the formal closing slide of your comprehensive Heart Failure presentation.
- The slide simply and clearly states "Thank you".
- The light blue background with floating squares maintains the clean, professional visual theme of the presentation .
Features of
Heart Failure Presentation
- Fully editable in PowerPoint
- All graphics are in vector format
- Medically Referenced information and data
 Slides count:
Slides count: Compatible with:Microsoft PowerPoint
Compatible with:Microsoft PowerPoint File type:PPTX
File type:PPTX Dimensions:16:9
Dimensions:16:9